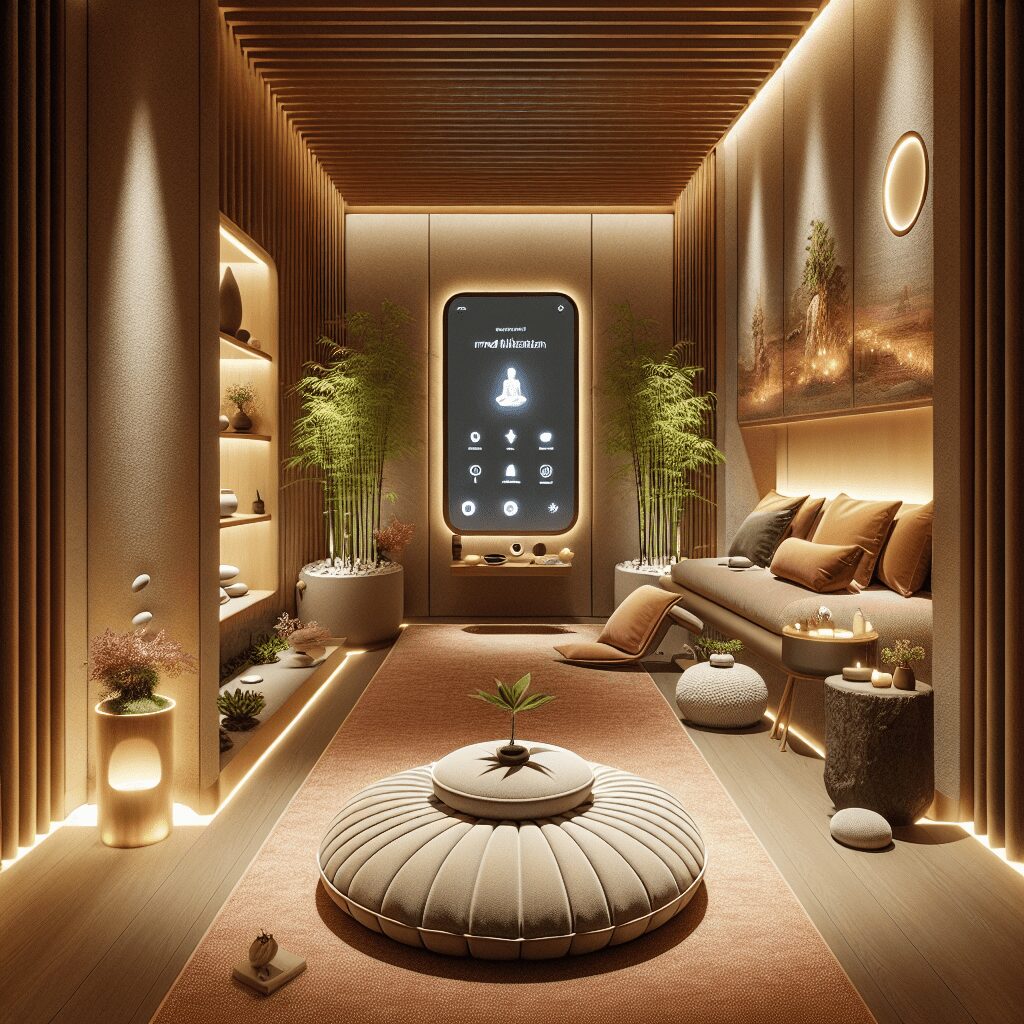
Prioritize your mental well-being daily. Enhance your life by nurturing your mental health with the Smart Meditation app. Break free from stress, alleviate anxiety, and enhance your sleep quality starting today.
How Long Does Xanax Stay In Breastmilk?
Navigating the Nuances of Xanax and Breastfeeding
When you’re navigating the transition into motherhood, the list of dos and don’ts seems never-ending, especially if you’re breastfeeding. Medications can be a particularly tricky area to navigate, and if Xanax is part of your healthcare regimen, you might be wondering: How long does Xanax, also known by its generic name alprazolam, linger in breastmilk?
Understanding the Half-Life of Xanax
Before diving into the specifics, understanding the concept of half-life is crucial. It’s a bit like knowing how long it takes for the last guest to leave a party – the half-life of a drug is the time it takes for its concentration in the blood to be reduced by half. For Xanax, this figure hovers around 11 to 16 hours. However, this doesn’t mean it waves goodbye to your system entirely in double that time; it takes roughly five half-lives for a drug to be considered significantly cleared from one’s system, translating to around 55 to 80 hours for Xanax. However, let’s add a cup of caution here: every body dances to its own rhythm, meaning metabolism rates can vary widely.
Xanax in Breastmilk: How Long Does It Stick Around?
When it comes to breastfeeding, the key concern is how much of the medication finds its way into the breastmilk and, subsequently, how much might be ingested by the baby. Recent studies throw a beam of light on this area, suggesting that Xanax does pass into breastmilk, but generally in small amounts. That said, ‘small’ doesn’t automatically mean ‘insignificant’. Infants, with their boutique-sized bodies and developing systems, can be more sensitive to these amounts.
Given Xanax’s half-life, it’s reasonable to deduce that it could be present in breastmilk for a few days post-ingestion. Yet, the exact timeline can be as clear as mud due to individual metabolic diversity. Factors like your metabolic rate, your baby’s age and health, and how much Xanax you’re taking all play pivotal roles in this biochemical production.
Minimizing the Risks: Tips and Tricks
If Xanax is a non-negotiable part of your healthcare plan, there are a few strategies you can employ to minimize risks for your little one:
-
Timing Is Everything: Try to time your doses just after feeding your baby or during their longer sleep stretches to allow time for the medication to metabolize before the next feeding.
-
Monitor Your Baby: Keep an eye out for any unusual symptoms in your baby, such as excessive sleepiness, feeding difficulties, or limpness. If you spot these, it’s time to ring up the pediatrician.
-
Open Lines of Communication: Always keep the dialogue open with your healthcare provider about your medication usage. They can offer tailored advice and might adjust your dosage or suggest alternative medications compatible with breastfeeding.
-
Consider Alternatives: If possible, explore alternative treatments with your healthcare provider that might have less impact on your breastmilk.
In Conclusion:
Venturing through the maze of breastfeeding while managing your health can feel like you’re trying to solve a Rubik’s Cube in the dark. If Xanax is part of your regimen, it’s not necessarily a hard stop on breastfeeding, but it does call for careful consideration and open communication with your healthcare team. By staying informed and vigilant, you can navigate this complex journey with a bit more ease, ensuring peace of mind for both you and your baby.