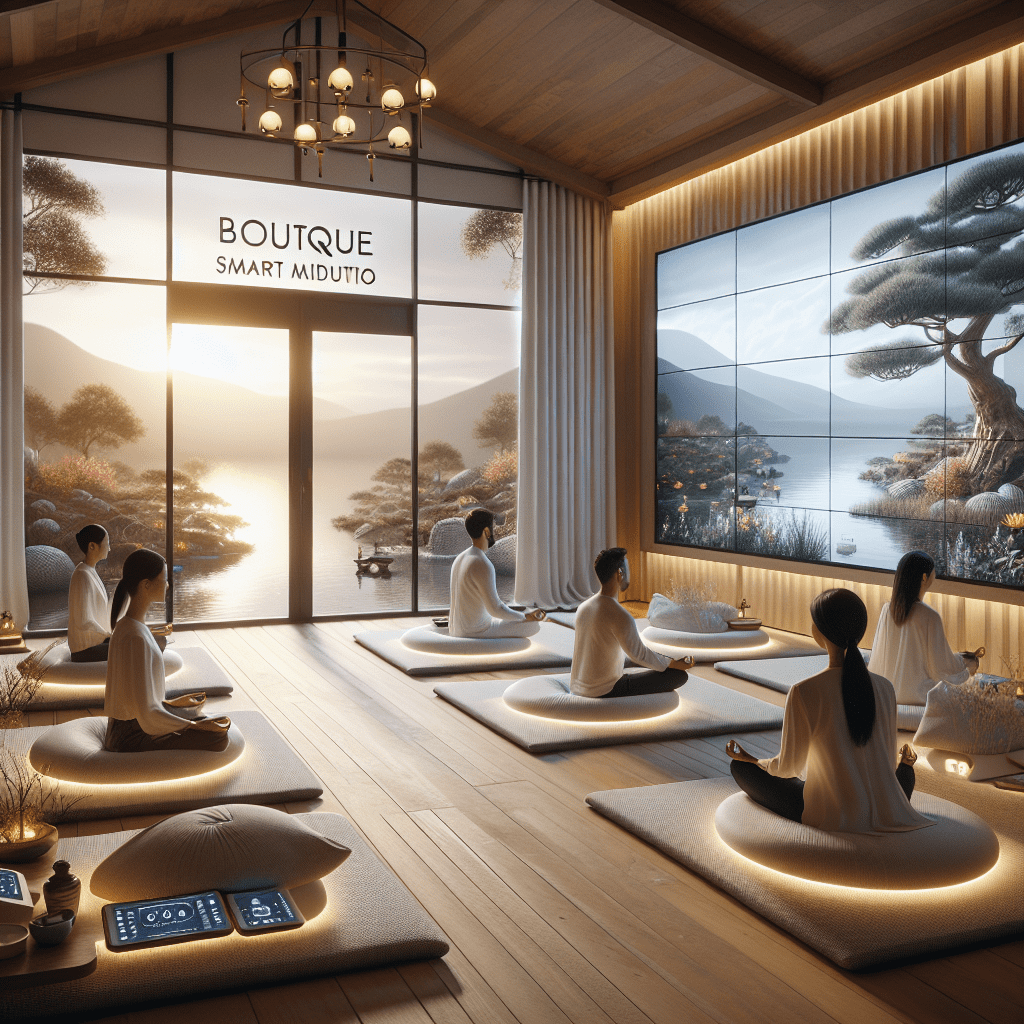
Prioritize your mental well-being daily. Enhance your life by nurturing your mental health with the Smart Meditation app. Break free from stress, alleviate anxiety, and enhance your sleep quality starting today.
How Do Doctors Decide Which Antidepressant To Prescribe?
Decoding the Prescription Process for Antidepressants
Navigating the realm of mental health can often feel like trying to find your way through a maze. When it comes to treating conditions such as depression, the array of available medications can indeed feel overwhelming. Ever wonder how physicians, those custodians of our health, make the call on which antidepressant to prescribe? Let’s dive into this intricate decision-making process, unmasking the method behind what may seem like medical mysticism.
The Art and Science of Choosing an Antidepressant
1. Understanding the Patient’s Unique Profile
It all starts with a story. A patient’s medical history is not just a collection of symptoms and episodes; it’s a narrative that holds the key to tailor-made treatment. Before a doctor even considers the medication aisle, they undertake a deep dive into:
- The nature of the depression: Is it a bout of major depressive disorder or a persistent depressive disorder?
- Medical history: Any pre-existing conditions can significantly influence the choice of medication.
- Concurrent medications: The pharmaceutical version of “too many cooks spoil the broth.” Some meds don’t play well together, and it’s crucial to avoid adverse interactions.
- Patient preferences and concerns: Some patients may prioritize medication that won’t add extra pounds, while others might be more concerned about insomnia.
2. The Mechanism of Action
Antidepressants are a mixed bunch, each wielding its magic in a slightly different way. Doctors often start with selective serotonin reuptake inhibitors (SSRIs), famously known for their fewer side effects. If SSRIs are the troupe dancers, consider serotonin and norepinephrine reuptake inhibitors (SNRIs) their back-up, often tapped for their dual-action prowess.
However, the plot thickens with the introduction of older classes like tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs), reserved for when other treatments have done the vanishing act on effectiveness. The choice hinges on how these medications interact with brain chemicals involved in mood regulation.
Beyond the Prescription Pad: A Collaborative Journey
Patient Follow-Up: The Pulse Check
Prescribing an antidepressant is far from a “set-it-and forget-it” scenario. Regular follow-ups are the compass that guides the treatment process, allowing for adjustments based on:
- Efficacy: “Is the medication lifting the fog of depression?”
- Tolerability: “Can the patient live with the side effects, or are they a deal-breaker?”
This iterative process is crucial, as the goal is not merely to alleviate symptoms but to restore the individual’s quality of life.
The Holistic Perspective: Beyond Pills
While medication is a frontline strategy, it’s part of a broader arsenal. Lifestyle modifications, psychotherapy, and self-care strategies form a multi-pronged approach, underscoring the fact that battling depression is more marathon than sprint.
Wrapping Up the Mystery
So there you have it. The selection of an antidepressant isn’t akin to throwing darts blindfolded. It’s a decision steeped in professional expertise, grounded in understanding the individual sitting across from the doctor. From evaluating the unique blends of symptoms and life circumstances to matching those with the medication’s profile, doctors navigate these waters with a blend of science, empathy, and personalized care.
Whether you’re navigating these choices yourself or supporting someone who is, remember: the journey to mental wellness is a collaborative odyssey. With open lines of communication and a pinch of patience, finding the right medication is a realistic and attainable goal.




