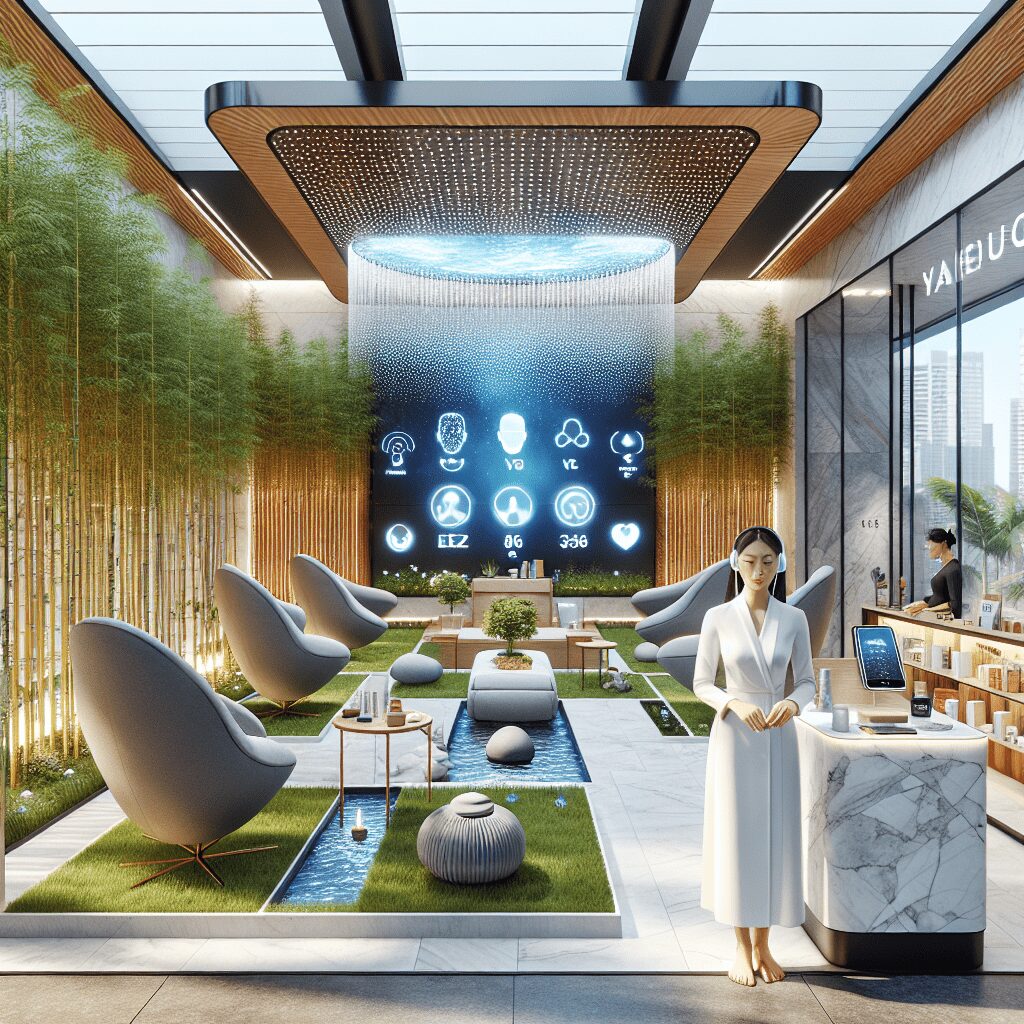
Prioritize your mental well-being daily. Enhance your life by nurturing your mental health with the Smart Meditation app. Break free from stress, alleviate anxiety, and enhance your sleep quality starting today.
Can Stopping Antidepressants Cause High Blood Pressure?
Navigating the Seas of Medication: The Link Between Antidepressants and Blood Pressure
In the intricate dance of mental and physical health, antidepressants often take center stage. They’ve been the knights in shining armor for many, battling the dragons of depression and anxiety. Yet, every knight has its armor chink, and for antidepressants, one such chink might just be its potential impact on blood pressure. The question at hand – can halting these meds cause your blood pressure to skyrocket? Let’s dive into the nitty-gritty and unravel this conundrum.
The Hidden Ripple Effect: Antidepressants and Blood Pressure Dynamics
Treading into the waters of antidepressant discontinuation, it’s essential to grasp how these meds play dice with your blood pressure. Antidepressants, particularly certain types, have a well-documented association with blood pressure changes. However, the plot thickens when you decide to cut the cord and stop taking them. Here’s the lowdown:
-
SSRIs and SNRIs: Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are like the high school popular kids of antidepressants – widely used and influential. They typically don’t cause a significant uptick in blood pressure when you’re on them. However, abruptly stopping them can lead to a sudden imbalance in neurotransmitters, potentially causing a spike in blood pressure as part of withdrawal syndrome or rebound symptoms. It’s like pulling the rug out from under your neurotransmitters, leaving them scrambling to regain balance.
-
Tricyclic Antidepressants (TCAs): On the other hand, TCAs are the old souls of antidepressants. They can directly increase blood pressure by causing the narrowing of blood vessels. While less commonly used today due to their side effect profile, the cessation of TCAs might reduce this risk – a silver lining, if you will.
-
MAOIs: Monoamine oxidase inhibitors (MAOIs), the vintage classics, can also hike up blood pressure, especially when you consume foods high in tyramine. Stopping MAOIs might decrease the risk of these hypertensive episodes, but as with any cessation, there are withdrawal risks.
Steering Through the Withdrawal Waters: What You Need to Know
Now, suppose you’re contemplating dropping the antidepressant anchor. In that case, it’s vital to do so under the guidance of a healthcare professional. Here are a couple of buoys to help you navigate these tricky waters:
-
Taper, Don’t Plunge: Rather than a full-stop, a gradual tapering off is the recommended route. It’s like acclimatizing to altitude changes – it gives your body time to adjust without going into shock.
-
Monitor, Monitor, Monitor: Keeping a close watch on your blood pressure during this period is crucial. Think of it as keeping an eye on the weather radar during a sea expedition. It helps in anticipating and managing potential storms (i.e., blood pressure spikes).
-
Lifestyle as Your First Mate: Embrace lifestyle adjustments as your trusty sidekick in managing blood pressure. Regular exercise, a balanced diet low in sodium, managing stress, and limiting alcohol can all be effective co-pilots.
In conclusion, while the relationship between stopping antidepressants and an increase in blood pressure is like navigating through a fog – complex and not entirely predictable – knowledge and preparation can serve as your lighthouse. Always consult with a healthcare provider before making any changes to your medication regime to ensure a safe and steady journey towards well-being. Remember, with the right maps and tools, navigating even the most perplexing waters becomes a voyage of discovery.